
Discover more from Fear of a Microbial Planet
But That Didn't Happen!
Ten examples where experts were wrong and/or common sense and evidence-based policies were dismissed.
Image: Shutterstock
As I was writing Fear of a Microbial Planet last year, I noticed some patterns emerge. Again and again, I found examples of instances where, in a rational world, the actions of authorities in response to COVID or other disease threats should be obvious, expected, and in the best interests of the public. However, in each instance, I was compelled to acknowledge reality and follow-up with “But that didn’t happen.” Because the response often wasn’t rational—it was mainly driven by politics and hysteria, and every irrational and non-evidence-supported act could be explained through this lens. As a result, the phrase is by far the most repeated in the book, and so I thought it would be interesting to compile ten examples of when a strong denial of reality ruled and common sense was abandoned.
The death of infectious disease, pre-1980s (Chapter 5):
In the years following World War II, improved sanitation, mass production of antibiotics and vaccines, and increased use of DDT resulted in plummeting death rates from infectious diseases in first-world countries. Filled with the confidence of these concrete successes, experts began to set goals for the eradication of many infectious diseases. Many books were published on the subject, including Man’s Mastery of Malaria in 1955 and The Evolution and Eradication of Infectious Diseases in 1963, all trumpeting the unlimited potential of technological innovations to wipe infectious disease from the earth once and for all.
But that didn’t happen. The advent of the AIDS pandemic in the 1980s killed the hubris of disease eradication, as it became more obvious that eradicated infectious diseases would simply be replaced by other diseases that were much harder to eliminate. The old, bad habits of centuries of epidemic responses, those driven by fear and ignorance and the blaming of others, returned, and habits that would lead to campaigns of disinformation, mass hysteria and germophobia have remained the norm for pandemics real and imagined ever since.
Media wildly exaggerating the risks of HIV infection among heterosexuals (Chapter 5):
It was the responsibility of health officials and scientists to inform the public about their risks of HIV infection, and it was the responsibility of the media to disseminate that information in a way that would empower individuals to make choices about their health without creating mass panic and irrational anxieties in those who had low risk of infection. But that didn’t happen. As Michael Fumento chronicled in his contrarian book The Myth of Heterosexual AIDS, six years after the first group of gay men with acquired immune deficiencies were identified, the risks of heterosexual transmission of HIV were still exaggerated and sensationalized. Oprah Winfrey, one of the most influential TV talk show personalities of all time, opened one of her shows in early 1987 with a panic-promoting monologue:
Research studies now project that one in five—listen to me, hard to believe—one in five heterosexuals could be dead from AIDS at the end of the next three years. That’s by 1990. One in five. It is no longer a gay disease. Believe me.
As you can probably guess, one in five heterosexuals were not dead by 1990. Not even close.
Embrace of COVID alarmists like Eric-Feigl Ding (Chapter 7):
Feigl-Ding has an extraordinary talent for making non-issues into issues, issues into crises, and crises into cataclysmic events of biblical proportions. How does he do it? He starts with emotive declarations in ALL CAPS. His first viral tweet on January 20, 2020, began with “HOLY MOTHER OF GOD!” He then referred to the reproductive number (which shows how fast the virus spreads) for the “new coronavirus is a 3.8!!!” That was completely misleading in the context of SARS-CoV-2, but the number more accurately reflected the growth of his Twitter followers, which spiked overnight as the tweet gained steam. His liberal use of emojis—including sirens, warning signs, and scared and crying faces, were well-placed to grab attention in every feed. Once his followers grew to hundreds of thousands, he began getting media coverage on CNN, MSNBC, and quoted in major newspapers. He was even recommended as a COVID expert by Twitter, with a recommendation appearing in the feeds of new users or anyone who searched for terms like “COVID-19” or “coronavirus”.
It gets worse. Feigl-Ding’s alarmist misinformation about COVID didn’t end with his first viral tweet. He tweeted about a preprint paper claiming to identify HIV-related sequences in the SARS-CoV-2 genome. The paper was quickly retracted, but not before meetings of Dr. Anthony Fauci and other high-level officials were called to discuss how to deal with the paper’s claims. He tweeted alarm about Mexico’s early 50% positivity rate of COVID testing, while ignoring the fact that testing was limited in Mexico to at the time to people who were seriously ill. He also confused virus reactivation with reinfection, a difference anyone that had taken a basic virology class would know.
On MSNBC, he made the patently absurd claim that the SARS-CoV-2 variant Omicron was more severe in children than in adults. Continuing his parent-targeting fearmongering, he championed public school closures, but went silent when his hypocrisy was exposed when it was made public that his wife and kids moved to Austria so that his children could attend in-person schools. He continued to make predictions about COVID death tolls that had no basis in reality, and was even publicly challenged by representatives of Denmark’s Statens Serum Institut for tweeting misleading graphs showing surges of deaths after COVID restrictions were lifted in Denmark in February, 2022. Some of his followers would defend him from these fact-based challenges with Twitter mob attacks and mass-trolling of his critics, thus discouraging many more public callouts of his constant stream of baseless and outlandish claims.
One would think that his expertise in infectious disease immunology would be carefully verified by media outlets before interviewing and labeling him an “expert.” But that didn’t happen. Feigl-Ding is an epidemiologist with an expertise in nutrition, not infectious disease. Although he did get his PhD from Harvard in 2007 after dropping out of medical school, his claims of being a “Harvard Epidemiologist” were based on an unpaid visiting-scientist appointment at Harvard in nutrition. His pre-pandemic expertise was in the health effects of diet and exercise, with absolutely no experience in pandemic or respiratory virus epidemiology.
The U.S. government pivots to exaggeration of COVID risks to scare people into changing their behavior (Chapter 7):
Now you might think that public health officials and leaders would see this widespread ignorance and misperception of risk and try to allay the public’s fears by providing clear and accurate information. But that didn’t happen. At least, it didn’t happen for long. For example, Dr. Anthony Fauci, director of NIH/NIAID’s early comments on COVID-19 to colleagues and the public were very matter-of-fact and much more reassuring than his later statements. On February 17th, he told USA Today’s editorial board, “Whenever you have the threat of a transmissible infection, there are varying degrees from understandable to outlandish extrapolations of fear.” On February 26, 2020, he told a CNBC panel “you can’t keep out the entire world” when asked about travel restrictions on inbound flights from China. Fauci also noted that while he thought China had been effective in containing the virus, they used methods which he called “draconian” that he doubted would be adopted in the U.S. The same day, he told CBS correspondent Dr. Jon LaPook in an email that, “You can mitigate the effects, but you cannot avoid having infections since you cannot shut off the country from the rest of the world.” He also warned against panic. “Do not let the fear of the unknown (i.e. a pandemic of a new infectious agent) distort your evaluation of the risk of the pandemic to you relative to the risks that you face every day. The only thing that we can do is to prepare as best as possible and do not yield to unreasonable fear.”
This is fantastic advice, and it would be hard to improve upon it! Dr. Fauci was clearly concerned about collateral damage caused by panic. However, the very next day he began to hedge a bit. In an email to actress Morgan Fairchild, who had worked with him during the 80s on HIV messaging, he wrote that community spread was becoming a problem in other countries, and might progress to a global pandemic. “If that occurs we will surely have more cases in the USA. And so for that reason, the American public should not be frightened, but should be prepared to mitigate an outbreak in this country by measures that include social distancing, teleworking, temporary closures of schools, etc.” He was also still concerned about irrational fear and panic. On February 29th, he told the hosts of the Today Show, “Right now, at this moment, there’s no need to change anything that you’re doing on a daily basis. Right now the risk is low.” Then he warned that things could change, “When you start to see community spread, this could change and force you to become more attentive to doing things that would protect you from spread.”
Very soon, community spread was confirmed. “Before there was a major explosion like we saw in the Northeastern corridor driven by New York City metropolitan area--I recommended to President Trump that we shut the country down,” Fauci told an audience at his alma mater, Holy Cross, later in October, 2020. Pressure from Fauci and White House Coronavirus Response Coordinator Dr. Deborah Birx eventually led to a press conference on March 16th, 2020, in which President Trump told the nation to shut down. When pressed upon the reason for the changes, Dr. Birx replied that “We’ve been working with groups in the United Kingdom. We had new information coming out from a model and what had the biggest impact in the model is social distancing, small groups, not going in public in large groups.” More specifically, a mathematical model from Imperial College-London was used that assumed that lockdowns would work, and unsurprisingly predicted that lockdowns would work and save millions of lives. A model that assumed a preventable catastrophe was all the maximizers needed to demand action.
A month later, Fauci would say that shutting down earlier could have saved more lives. Later in the year, he would lament that the U.S. didn’t shut down more stringently, “Unfortunately, since we did not shut down completely the way China did, the way Korea did, the way Taiwan did, we actually did see spread even though we shut down.” As I mentioned earlier, places that shut down also saw massive collateral damage, which would have been even worse in the U.S. if the preferred “draconian” response had been implemented.
Many other places implemented incredibly harsh lockdowns that failed even more miserably. Peru, for example, had one of the harshest lockdowns in the world, and was rewarded for it with one of the highest death rates. Most of South America had a very hard time with COVID outbreaks, as did North America and most of Europe, while most of Asia did not, despite differences in mitigation efforts. I will get more into pandemic response scorekeeping in Chapter 13, but suffice it to say, lockdowns weren’t the panacea the maximizers claimed they would be.
Once committed to shutting down a country without much evidence the benefits will outweigh the costs, leaders and health officials will become keenly aware of any confirmation that they made the right decision, and equally resistant to any disproof. In the United States, state leaders were ultimately responsible for pandemic policies, and this ensured there would be 50 different strategies and outcomes for comparison. Unsurprisingly, most media outlets favored the most draconian responses. The more people were isolated at home, grasping for every bit of terrifying information they could get, the better.
Predictions of doom for reopening states (Chapter 7):
Among U.S. states, there were clear gaps in policies. Some continued stay-at-home orders much longer than others, mandated masks in public and schools, and kept “non-essential” businesses closed for months. Only one state, South Dakota, never closed or issued mandates. Others opened up after the initial wave passed and never closed again. Georgia’s Governor Brian Kemp announced on Monday, April 20th that the state would reopen on April 27th. This announcement was not well-received. “Georgia’s Experiment in Human Sacrifice” blared a headline in The Atlantic two days later. Fortunately, the article itself was less over the top than the title. It profiled business owners that were scared to open, quoted multiple bipartisan critics, and cited Georgia’s lousy testing capacity and recent outbreaks as reasons it was courting certain catastrophe.
But that didn’t happen. Cases actually decreased after Georgia reopened, and didn’t spike again until the end of June, 2020, when cases simultaneously surged all over the south, regardless of policies. Florida, which unlike Georgia had very few cases prior to shut down, otherwise had a similar experience, with Governor Ron DeSantis announcing a phased reopening starting on May 4th. Critics had blasted Florida’s response, which didn’t kick in until April 1st, after thousands of college students had mobbed Florida’s beaches during Spring Break. “Florida’s governor keeps hitting new lows in the battle against the coronavirus,” scolded CNN editor Chris Cillizza. The Miami Herald was equally exasperated with DeSantis’s failure to get with the program, with an editorial titled “We’re looking like ‘Flori-duh’ again, Gov. DeSantis. Any idea how that happened?” However, keeping the state open appeared to have no immediate consequences, for which a CNN article explained, “luck may have been a factor,” and that scientists were “puzzled” that there weren’t more deaths. Like Georgia, Florida had a surge in cases in June, as did Texas, South Carolina and Mississippi. DeSantis made clear his disdain for pandemic models and the draconian responses they promoted in other states, and vowed by the end of August that “We will never do any of these lockdowns again.”
Similar pandemic outcomes in terms of cases, hospitalizations, and deaths would continue to puzzle scientists who believed that the assumptions of their models were correct. They would continue to point to outliers of places that had low numbers of deaths, like the Pacific Northwest, Vermont, and Hawaii, and continue to explain their “success” purely by policies, while continuing to ignore geographic and demographic differences, as well as places like California, which had very strict mitigation policies and had a similar age-adjusted outcome as Florida.
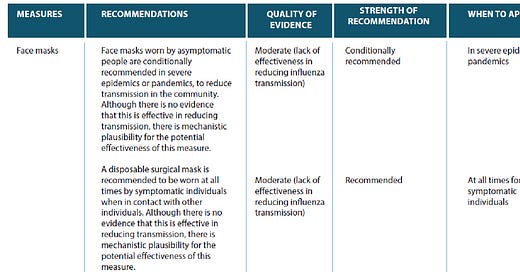
CDC’s failure to make recommendations based on evidence (Chapter 8):
Perhaps sensing they were losing a war with reality, the CDC release a document titled “The Science of Masking to Control COVID-19.” The CDC brass must have thought this document would help their case. Instead, for people that cared about evidence (admittedly a shrinking group) it had the opposite effect. The document was a tour-de-force of low-quality ecological and controlled lab studies that only demonstrated weak correlation with the real world. But that didn’t stop the CDC from wrapping it in a bow with a shiny “CAUSATION!” label.
It was even worse than that. Many of the references only examined the mechanics of small aerosol/airborne particles and large droplet emissions and did not assess the efficacy of masks. Of the other cited references, many offered conclusions that did not support universal cloth masking as source control for aerosol/airborne transmission in asymptomatic individuals, which was only acknowledged by the CDC as “potential” route of SARS-CoV-2 spread. However, the CDC was wrong about this, too--it had already been suspected in June of 2020 that aerosol was the predominant mode of transmission, and environmental engineers/aerosol experts had been subsequently pushing for recognition of airborne transmission as a major route of SARS-CoV-2 transmission. Thus, when CDC-cited authors like Bandiera et al stated their concern “If the aerosol transmission is later determined to be a significant driver of infection, then our findings may overestimate the effectiveness of face coverings,” the CDC had a responsibility to acknowledge the effect of new evidence on their recommendations. That didn’t happen.
The CDC’s pro-mask document even cited the Rengasamy study as supporting evidence, despite the authors conclusion that cloth masks were useless, as I cited at beginning of this chapter. Additional references to the Missouri hairstylist “study” and an anecdote of a single, symptomatic, masked passenger failing to infect others on a 15-hour flight from Wuhan to Toronto really called into question—what the hell were they thinking? Yet this was the standard to which the CDC was held, especially by lapdog media outlets regarding evidence of mask efficacy during the pandemic. They could’ve written the document in crayon and it wouldn’t have changed a thing.
Outright hostility to the results of DANMASK-19 (Chapter 8):
Despite the dearth of controlled real-world studies of mask efficacy in prevention of SARS-CoV-2 community spread, and a complete lack of interest by U.S. government agencies in filling that void, a research group in Denmark stepped in. The first randomized control trial, dubbed DANMASK-19, with 6,000 participants, enrolled employees in a Danish grocery store chain, with half of the participants wearing masks and the other half unmasked. This study was completed in June of 2020.
Yet by October, it was clear that something was wrong. Despite being of intense interest and of obvious high impact, that study had not yet been published. Surely the data analysis had been quickly completed and the paper had been submitted to a top journal for review? Given the nature of the study, it would also make sense that the editors would make every effort to get the study reviewed as quickly as possible and, if the methods were acceptable and conclusions supported by the data, publish without delay.
But that didn’t happen. An article published in a Danish newspaper revealed that the authors had submitted the paper to three top journals, The Lancet, The New England Journal of Medicine, and the Journal of the American Medical Association. All three had rejected the paper, and the authors insinuated that the rejections were political in nature. They refused to comment more specifically, noting that they were unable to comment without revealing the results of the study. Interestingly, even before publication, the authors were pressed to defend their methodology, insisting that they were only able to assess the incidence of infection among mask-wearers, and not the incidence of infection among their contacts (i.e. source control).
Lack of skepticism of conclusions of Bangladesh mask study (Chapter 8):
In September, 2021, an early Christmas miracle happened—the results of a cluster-randomized controlled trial conducted in villages in Bangladesh reported fewer infections in masked villages than in unmasked villages. In response, hopeful media outlets worldwide climbed the nearest snow-capped mountain, joined hands and began to sing:
“Largest study of masks yet details their importance in fighting Covid-19.” –NBC News
“We Did the Research: Masks Work, and You Should Choose a High-Quality Mask if Possible.” –The New York Times
“Massive randomized study is proof that surgical masks limit coronavirus spread, authors say.” –Washington Pos
“Studies support use of face masks in limiting spread of COVID-19.” – Associated Press
“Face masks for COVID pass their largest test yet.” --Nature
“Masks are effective’: Stanford Medicine study finds surgical masks help prevent COVID in Bangladesh.” –SF Gate
“Huge, gold-standard study shows unequivocally that surgical masks work to reduce coronavirus spread.” –LiveScience
I could go on, but you get the idea. This was the evidence all those desperate for high-quality, “gold standard,” and bias-confirming studies were waiting for. The lead author, economist Jason Abaluck, confidently told the Washington Post “I think this should basically end any scientific debate about whether masks can be effective in combating COVID at the population level.”
That didn’t happen. Within a few hours, critics on social media began to poke considerable holes in the study’s conclusions and methodology. This was a slower process that wasn’t going to result in the same high-fiving, click-bait stories, but was necessary nonetheless.
First of all, the study had an important negative result—there were no differences seen for cloth masks, only surgical. Most people at the time were wearing cloth masks. After all, the CDC had pushed them loudly and consistently. Yet this study showed no benefit for cloth masking.
Second, the results were age-stratified. Surgical masks seemed to work only for people over 50. Why on Earth would that be the case? That wasn’t necessarily a result of “masks working”. Maybe older people were more likely to self-report what the researchers wanted to hear. Masks were heavily promoted in the experimental villages. Could that not affect other behaviors? In fact, it did affect other behaviors, as the authors reported that social distancing increased in mask-promoted villages.
Third, the authors didn’t provide any useful information about past case or testing rates for the villages. This makes it almost impossible to accurately compare changes, especially if conclusions rely on self-reported data.
Fourth, they claimed an 11% reduction in cases in masked villages, with confidence intervals that ranged from 18% to 0%. You read that correctly. Zero was still a possibility.
Fifth, the differences the authors claimed were based on a difference of 20 cases out of more than 340,000 people, with 1,106 seropositive individuals in the control group and 1,086 in the mask group. They didn’t mention this anywhere in the original paper, for obvious reasons.
Sixth, they didn’t make their data and full code immediately available for others to analyze. This would put some questions about massaging their statistics for a favorable outcome and immediate fame to rest. To their credit, they did eventually do this. This allowed Maria Chikina and Wes Pegden of Carnegie-Mellon and Ben Recht of UC-Berkeley to re-analyze the raw study data and ultimately find no significant differences based on masking. Instead, they found that more significant differences in physical distancing and concluded that “behavior of unblinded staff when enrolling study participants is one of the most highly significant differences between treatment and control groups, contributing to a significant imbalance in denominators between treatment and control groups.” In other words, the study was hopelessly biased and confounded from the beginning. Not exactly a ringing endorsement of universal masking. Needless to say, media people were not screaming this alternate explanation from the top of a mountain, a roof, or of anything.
Refusal to acknowledge biases towards exaggerated COVID harms (Chapter 11):
The overwhelming desire for evidence of interventions that effectively eliminate the risk of infection will inevitably pressure scientists to provide that evidence. Ideally, an acknowledgement of this bias would result in increased skepticism from other scientists and media outlets. Clearly, that didn’t happen, and exaggerated claims of efficacy of interventions and exaggerated harms of COVID to promote their acceptance became the norm in pandemic reporting.
The best way to mitigate research bias is for investigators to invite neutral partners to replicate work and collaborate on additional studies. The ability to make all data available to the public and other scientists also invites critical reviews that are crowd-sourced and thus potentially more accurate and less biased. Public availability of datasets and documents resulted in the improvement of pandemic forecasting by independent analysts like Youyang Gu and brought the possibility of a lab-leak origin for SARS-CoV-2 out of conspiracy-theory shadows and into public light.
Failure of epidemiological models (Chapter 12):
The behavior of the virus in different places seemed to defy many epidemiological models, as waves of cases seemed to peak before they were predicted to peak, leaving a lot of people that were still susceptible. Many of the models predicted a compressed pandemic where everyone was completely susceptible and most would be infected in a short period of time without serious community-wide mitigation efforts. Models also predicted that when restrictions were lifted, cases would surge fairly quickly (e.g. Georgia’s “experiment in human sacrifice”).
But, as I’ve grown used to writing, that didn’t happen. Epidemiological models couldn’t explain why places with seroprevalence at 10% or even lower and low community restrictions weren’t experiencing cataclysmic surges of infections. That’s when, like everything else in the pandemic response, the immune system got politicized.
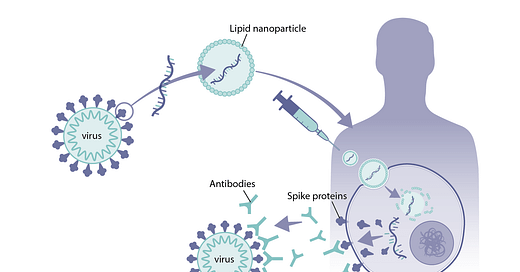
Bonus: Exaggeration of COVID vaccine benefits (Chapter 12).
Now one might think that infections exploding in COVID-vaccinated populations would cause government officials to alter their rhetoric regarding vaccine benefits and their recommendations. However, although I didn’t specifically write the phrase in FMP, that didn’t happen:
In the first few months after the SARS-CoV-2 mRNA vaccines became available, it was clear they were successful in preventing hospitalizations and deaths. By the spring of 2021, many hospitals were reporting that their COVID patients were largely unvaccinated. Prevention of hospitalization in people older than 65 by the Pfizer-Biontech (96%), Moderna (96%), and J&J (84%) vaccines was later confirmed by analysis of U.S. hospital databases. The efficacy of COVID vaccines was also evident in Israel, the first country that achieved the high levels of vaccination coverage for adults, with a hundred-fold decrease in infection rates in May 2021 compared to the peak months earlier.
However, one month later, in June, Israel experienced another COVID outbreak, this time in both vaccinated and unvaccinated individuals. By August, Pfizer and Moderna had released data indicating that reinfections were more common in vaccinated groups than in the more recently vaccinated placebo groups. Sterilizing immunity to the widely distributed SARS-CoV-2 mRNA vaccines was waning after only a few months.
Spikes of reinfections months after mass vaccination campaigns was contrary to what public health officials and politicians had very recently claimed. “When you get vaccinated, you not only protect your own health and that of the family but also you contribute to the community health by preventing the spread of the virus throughout the community,” Anthony Fauci had said in a May 2021 interview on CBS’s Face the Nation. “In other words, you become a dead end to the virus,” he added. On MSNBC in March, Rochelle Walensky had claimed that “our data from the CDC today suggests that vaccinated people do not carry the virus.” Not to be outdone, President Joe Biden said at a CNN town hall in July 2021 that "You’re not going to get COVID if you have these vaccinations." To be fair, Fauci and Walensky were in a gray area in March and May of 2021 and could’ve just been naively hopeful about the long-term efficacy of COVID vaccines. However, by July, Biden’s statement was demonstrably false.
So many “break-through” infections just months after vaccination presented a political problem. At first, the easiest route for any politician was to pretend that reinfections weren’t happening, or that they were super rare. As more outbreaks occurred in highly vaccinated populations, reality became impossible to dismiss. The Biden administration had supported vaccine mandates, and attempted to enact a nationwide mandate, which was eventually watered down to military personnel, government funded healthcare centers, and foreign travelers to the U.S. However, vaccine mandates were also enacted in twenty-one states, many municipalities, and in hundreds of corporations, including universities. With thousands of breakthrough infections reported, the rationale behind these mandates evaporated along with the idea that “your vaccine protects me.” This was especially problematic for the many healthcare providers that had fired staff for refusing COVID vaccination, the same ones that later experienced crippling staff shortages for no long-term benefit.
Another significant problem for vaccination efforts lay in the numbers of adverse events reported on publicly available databases such as the Vaccine Adverse Event Reporting System (VAERS). VAERS is the largest post-market surveillance database for reporting of adverse events that occur after vaccination. The CDC website calls VAERS “the nation’s early warning system,” yet cautions that “a report to VAERS does not mean that a vaccine caused an adverse event.” That’s because anyone can submit a report—only the more serious cases or patterns in the reports are further investigated. Due to mass vaccination with COVID-19 vaccines in a short period of time, VAERS reports were likely to spike regardless of actual risks. Bad things happen to a lot of people each year, and sometimes it is just a coincidence that it happens after a vaccination. The key to investigating these patterns is calculating these events in the context of their baseline levels, and considering all other possible causes.
These considerations didn’t stop vaccine skeptics and antivaxxers from seizing on the data as proof of the hazards of COVID vaccination. After all, if every adverse event after COVID infection could be attributed to COVID, why not every adverse event after vaccination? In these cases, extreme positions were easy to spot, as both antivaxxers and vaccine militants tended to completely dismiss the importance of one type of event and consistently amplify the other.
Yet it was true that the COVID vaccines had bypassed the traditional FDA approval process, which includes extensive safety monitoring, and thus it was likely that many potential adverse effects had been missed or downplayed by vaccine manufacturers in the rush to emergency approval. Unfortunately, U.S. government agencies didn’t seem interested in supporting studies to further investigate adverse effects of COVID vaccines. That responsibility was left to other countries.
By mid-2021, the most significant adverse effect of COVID mRNA vaccines was myocarditis (heart inflammation and possibly scarring), observed mostly in young males. This was especially true of the Moderna vaccine, as data from Scandanavian countries and France found rates in Moderna recipients to be 3-4 times that of Pfizer recipients. By the fall of 2021, enough evidence had accumulated to convince many northern European countries to restrict the use of the Moderna vaccine in people under 30 years of age. For older individuals, the benefits of the Moderna vaccine continued to outweigh the costs. The Pfizer-Biontech vaccine was not without a reported possibility of myocarditis in young males, as a 2022 study in Thailand found myocarditis in 3.5% of males aged 13-18 years, particularly after the second dose. Pfizer vaccination was also not recommended for children in many European countries, especially those 0-11 years of age, due to a lack of evidence of a clear benefit.
These countries weren’t being overtaken by antivaxxers, they were simply performing cost/benefit analyses, and finding the benefits of COVID vaccines to not be significantly larger than the potential costs, particularly for young children and teenage males. However, the CDC didn’t come to the same conclusions, continuing to recommend COVID vaccines for children older than 6 months of age, and boosters for those 5 years and older, as late as the fall of 2022, despite accumulating evidence of vaccine-associated myocarditis/pericarditis in young people. The reason for the gap in the CDC and European recommendations wasn’t clear, although the most obvious simply involves following the money.
Unfortunately, many of these examples are not becoming outdated. Mask mandates have returned in some places, including schools, despite no high-quality supporting evidence. Same for COVID vaccine booster recommendations for healthy people under 65. Many European countries, including Denmark, have altered their recommendations based on careful risk/benefit analyses. Once again, although it would seem obvious that U.S. leaders should have followed suit, that didn’t happen.
Subscribe to Fear of a Microbial Planet
Fighting back against a germophobic safety culture.













"By the spring of 2021, many hospitals were reporting that their COVID patients were largely unvaccinated."
For the US, at least, I'm not sure that data was available to draw that conclusion. The system for registration of COVID and other vaccination in the US is Byzantine and classification of the COVID vacciantion status throughout much, if not all of the pandemic was unreliable. https://kffhealthnews.org/news/article/huge-gaps-in-vaccine-data-make-it-next-to-impossible-to-know-who-got-the-shots/
On the other hand, federal registration of population rates of vaccination was probably near complete or even overestimated leading to relatively accurate or even overestimation of the rates of COVID vaccination.
This gives rise to what I would refer to as the two-sets-of-books bias. It is likely that, while the CDC surveyed the state registries for the relative rates of hosptalization/deaths in the unvaccinated vs vaccinated, the "denominator data" of the local population rates of vaccination were derived from the more complete federal COVID vaccination database. This is stated explicitly in a CDC COVID-NET publication: https://www.medrxiv.org/content/10.1101/2021.08.27.21262356v1.full.pdf (Supplementary figure 3).
This bias may explain, in part, the claims of the CDC of 66% efficacy of COVID vaccination against all-cause mortality. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8553028/pdf/mm7043e2.pdf
Summarizing: the claim of efficacy of COVID vaccination severe disease and death is a central tenet of public health authorities, but it is less certain than commonly believed.
Excellent thank you for this digestible summary.